Old Process Overview:
Previously to April 1, 2013, providers would
submit bills to the county, who would pay the providers upfront. The county would then try to collect
reimbursement from insurance companies and Medicaid.
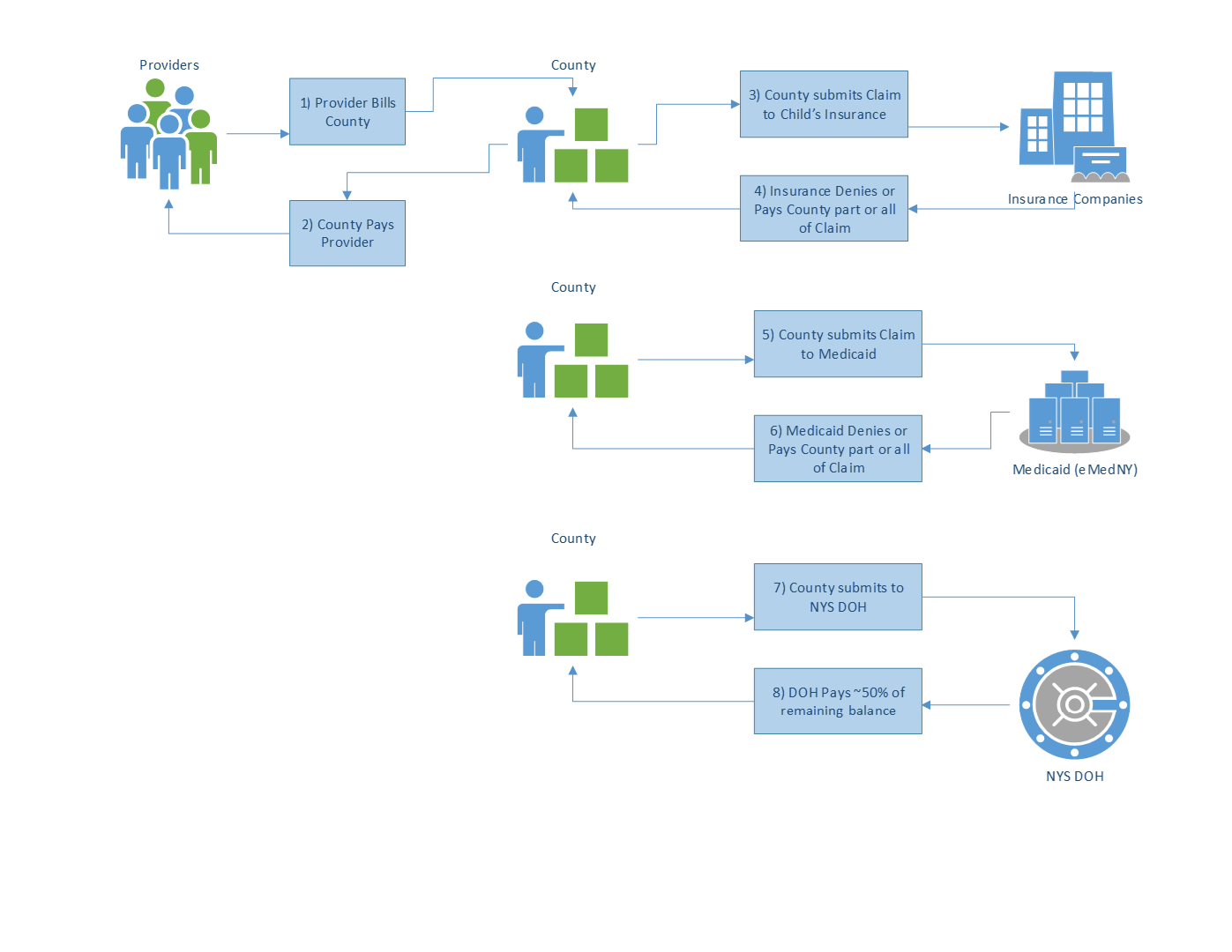
New Process Overview:
In 2012, as part of the budget, NYS enacted a change whereby
providers would first seek reimbursement from commercial insurance, then
Medicaid, and finally the county would be the payer of last resort. The change also provided for the Department
of Health to implement a Fiscal Agent (FA) to manage the claiming and
reimbursement process for providers.
With this new model, claims will still need to pass edit
checks in KIDS and NYEIS, but claims submitted via KIDS or NYEIS are forwarded
to the Interim Fiscal Agent System (IFSA) to manage the claiming and
reimbursement process for providers. The
IFSA will first try to bill any commercial insurance a child has, then
Medicaid, and any remaining balance on a claim will be paid out of the
county-funded state escrow account.
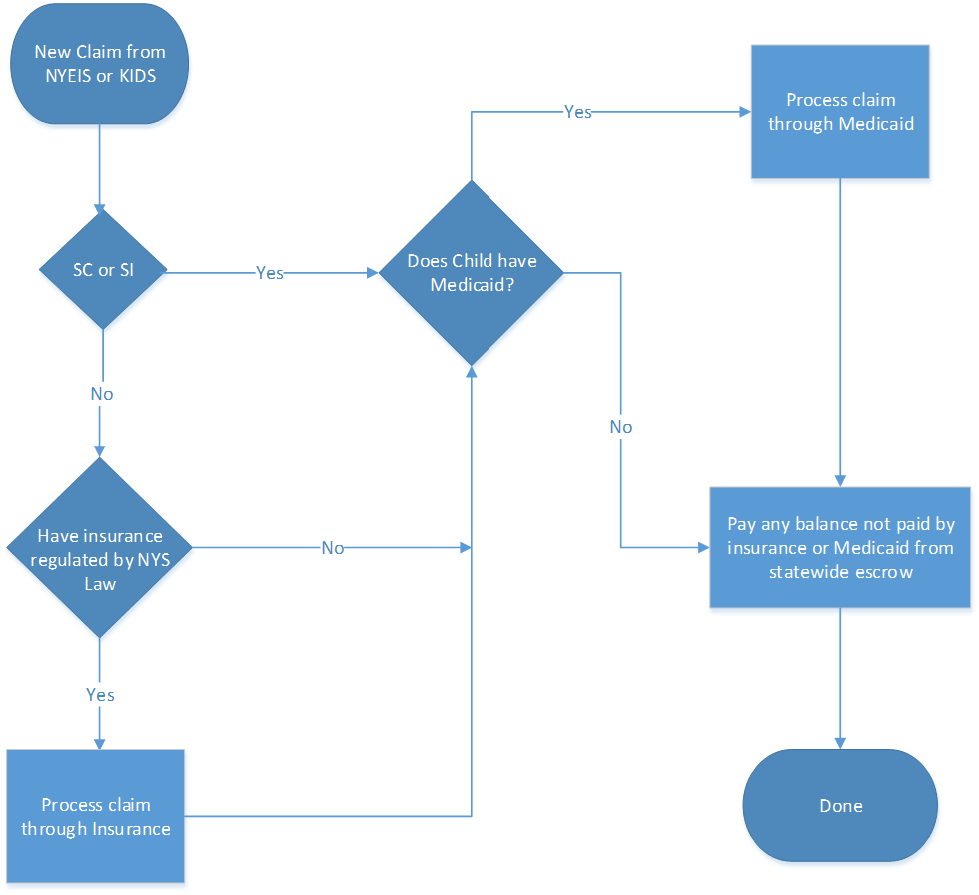
Insurance:
The IFSA will only bill insurance companies or policies that
are regulated by NYS insurance law. If a
child does not have insurance or the insurance is not regulated by NYS, the
claim will move forward to Medicaid.
Insurance companies will not be billed for service coordination or
special instruction – these claims will move forward to Medicaid. If a child has multiple insurance policies
(ex: covered by two parents), all claiming against all policies will be
attempted. Providers will receive
payment via check directly from insurance companies. Depending on the company, this process of
billing and waiting for a response can take time.
Medicaid:
The IFSA will receive a CIN number for all Medicaid eligible
children from KIDS or NYEIS. All
services for children with a Medicaid CIN will be claimed to Medicaid. If a child does not have a Medicaid CIN, the
claim will move forward to the county funded escrow account. Providers will receive payment from Medicaid
via check or electronically, depending on the provider.* Response and payment
from Medicaid are timely and predictable.
For more information, see the Medicaid Cycle.
*If you wish to receive payment electronically, you need to
enroll with eMedNY for an EFT.
County Escrow
Account:
The remaining balance of a bill will be paid out of the
county-funded state escrow account. The
IFSA will do a bi-weekly sweep for outstanding claims and request that the
state issue payment to providers.
Counties will be responsible for depositing reimbursement to the escrow
account. Providers will receive payment
via check directly from the escrow account.
Article ID: 54, Created On: 5/7/2013, Modified: 10/28/2015